Key Takeaways from the Regulatory Affairs Professional Society (RAPs) EuroConvergence 2025

This blog was originally posted on 21st May, 2025. Further regulatory developments may have occurred after publication. To keep up-to-date with the latest compliance news, sign up to our newsletter.
AUTHORED BY FERNANDA PARO, REGULATORY COMPLIANCE SPECIALIST, COMPLIANCE & RISKS
RAPs EuroConvergence 2025 offered valuable insights and was packed with rich content on the MedTech sector. Below are some of the interesting key topics that were discussed.
The European Commission’s opening remarks at the event highlighted the strong link between regulatory changes, innovation, and competitiveness in the EU medtech industry. Current work includes a targeted evaluation of the Medical Devices Regulation (MDR) and the In-vitro Diagnostic Regulation (IVDR), along with planned initiatives to simplify regulations, improve Notified Body consistency, broaden the definition of Well-Established Technologies1, support innovation for orphan and pediatric devices and breakthrough technologies, and encourage e-IFUs (electronic Instructions for Use) for sustainability.
The main point was that regulatory flexibility and competitiveness are connected, requiring stakeholders to be proactive as the EU shifts towards a more innovation-driven regulatory environment during 2024–2029.
AI/ML in MedTech: A U.S. Regulatory Perspective
As artificial intelligence and machine learning (AI/ML) technologies continue transforming the healthcare and medical device sectors, the U.S. regulatory framework is evolving to keep pace, balancing innovation with patient safety and public trust.
Eric Henry, Senior Quality Systems & Compliance Advisor, offered a detailed overview of the current and emerging U.S. regulatory environment for AI/ML-enabled medical devices.
The presentation mapped a comprehensive and fast-evolving landscape of regulatory touchpoints, including:
- AI/ML PCCP Guidance (FDA)
- Draft AI/ML medical device lifecycle guidance (FDA)
- Content of Premarket Submissions for Device Software Functions Guidance (FDA)
- Clinical Decision Support Software Guidance (FDA)
- Digital Health and Artificial Intelligence Glossary (FDA)
- Health Data, Technology, and Interoperability-1 (P-DSIs) (45 CFR Part 170 / 171) Final Rule (ASTP/ONC)
- Health Data, Technology, and Interoperability-2 (TEFCA) (45 CFR Parts 170 / 171 / 172) (ASTP/ONC)
- Federal Trade Commission (FTC) Act – Section 5 – (and accompanying guidance)
- AI Risk Management Framework (NIST)
- GMLP for Medical Device Development: Guiding Principles (FDA, Health Canada, MHRA)
- PCCP for ML-Enabled Medical Devices: Guiding Principles (FDA, Health Canada, MHRA)
- Transparency for Machine Learning-Enabled Medical Devices: Guiding Principles (FDA, Health Canada, MHRA)
- Safe, Secure, and Trustworthy Development and Use of Artificial Intelligence (EO 14110) (White House)
- Design controls and software guidelines, and Standards (FDA, AAMI, IMDRF, IEC, ISO, etc.)
- State-level AI and privacy legislation (e.g., California, Colorado, Utah)
The panelist also pointed to several emerging trends that are expected to shape future regulatory approaches to AI in the life sciences. These include the integration of AI-specific criteria into quality system regulations, increased linkage between cybersecurity and AI/ML in FDA guidance (such as for Clinical Decision Support tools), and potential enforcement actions like “algorithmic disgorgement2” by the FTC.
We can also anticipate wider adoption of standards from bodies like AAMI, IMDRF, and IEC, more state-level privacy laws, greater Department of Justice (DOJ) scrutiny, and further development of frameworks like the NIST AI Risk Management Framework for generative AI.
While current regulations are generally effective for locked algorithms3 , the session emphasized the growing need for more adaptive oversight, especially for AI/ML systems.
In addition, another key focus was the Predetermined Change Control Plan (PCCP), a concept designed to accommodate the evolving nature of machine learning while ensuring safety and effectiveness. PCCPs aim to streamline regulatory processes by allowing certain pre-defined changes without requiring new submissions, as long as robust validation and risk management are in place.
Navigating the Intersection of MDR and HTA: Strategic Implications for Medical Device Manufacturers
In this panel, Dr. Thomas Miramond of NAMSA highlighted a pivotal shift in the EU regulatory landscape: the increasing integration of the Medical Device Regulation (MDR) and the Health Technology Assessment (HTA) Regulation.
This shift calls for medical device manufacturers to move away from siloed, sequential evidence planning and toward a harmonized approach that serves both regulatory approval and reimbursement goals.
MDR provides the clinical groundwork, focusing on device safety, performance under intended conditions and the clinical benefit and overall benefit-risk ratio. HTA expands the evidence framework to include: 1) comparative effectiveness, evaluating how a device performs against alternatives; 2) Health economics, assessing cost-effectiveness and budget impact; 3) Societal and ethical implications; and 4) Real-world evidence (RWE) and long-term health outcomes.
This broader scope means manufacturers must consider study designs aligned with PICO principles (Population, Intervention, Comparator, Outcome), select comparators meaningful to payers, and focus on endpoints that reflect both clinical relevance and economic value.
To ensure timely and successful market access in the EU, manufacturers must align their clinical evidence strategies early on, not just to satisfy regulatory requirements, but to support HTA evaluations that determine reimbursement and market viability.
Impact of the Battery Regulation (EU) 2023/1542 on Medical Devices
The regulatory landscape in the EU keeps evolving. With Battery Regulation (EU) 2023/1542 entry into force in August 2023, the European Commission has introduced a new lifecycle-based framework that significantly reshapes battery compliance requirements across sectors. For the medical technology industry, this regulation is not just another legal update, it’s a call to action.
Unlike its predecessor, the new regulation explicitly includes batteries integrated into products, which means that many medical devices are now squarely in scope. From diagnostic equipment and wearable monitors to rechargeable surgical tools and home-health devices, manufacturers must now prepare for a wider set of obligations.
From a MedTech perspective, this isn’t just about environmental compliance, it’s about design, documentation, market access, and sustainability strategy. And for companies already navigating the complexities of the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), the overlap is significant.
To avoid duplicated efforts, or worse, compliance gaps, manufacturers must harmonize their regulatory strategies, including the new procedures involving Conformity Assessment and CE Marking, Documentation/Labelling, Design and others.
In addition, in terms of End-of-Life & Sustainability, they also must consider collection, recycling, and Extended Producer Responsibility (EPR). These obligations impact logistics, distribution, and post-market surveillance systems.
Borderline and Drug-device Combination Products
The EU is working to better coordinate the regulation of borderline and combination products that fall between medicines and medical devices. While national competent authorities (NCAs) handle initial classifications, complex cases may involve EU-level input, including support from the European Medicines Agency (EMA).
Proposed pharmaceutical legislation would expand EMA’s role in offering scientific recommendations and promoting cross-framework collaboration. A key challenge remains avoiding duplication between EMA/National Competent Authorities (NCAs) and Notified Bodies in assessing these products. NCAs currently offer an EU-wide opinion through the Helsinki procedure, and EMA provides support with classification of borderline products (e.g Innovative Task Force (ITF)).
The effective development and regulation of combination products in the EU depend on a predictable, integrated framework that supports both innovation and patient safety. Ongoing efforts, such as the COMBINE initiative4, multidisciplinary scientific advice, and enhanced procedural alignment are key to ensuring consistency in the evaluation of clinical and performance data while reducing regulatory overlap. With continued guidance from the EMA, including on Article 117 MDR and variation classifications, and reinforced collaboration across regulatory bodies, the EU is steadily building a multidimensional, future-ready regulatory environment that meets the complex needs of combination products.
Stay Ahead Of Regulatory Changes in Medical Devices
Want to stay ahead of regulatory developments discussed at RAPs EuroConvergence 2025?
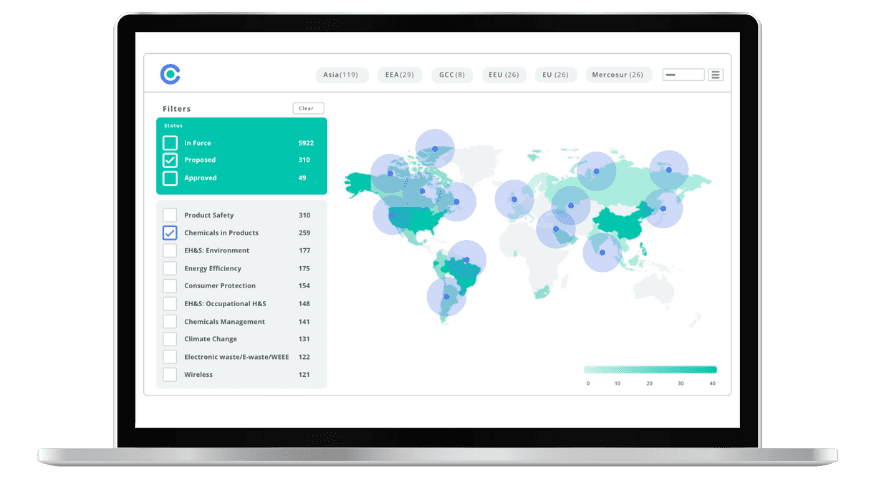
Accelerate your ability to achieve, maintain & expand market access for all products in global markets with C2P – your key to unlocking market access, trusted by more than 300 of the world’s leading brands.
C2P is an enterprise SaaS platform providing everything you need in one place to achieve your business objectives by proving compliance in over 195 countries.
C2P is purpose-built to be tailored to your specific needs with comprehensive capabilities that enable enterprise-wide management of regulations, standards, requirements and evidence.
Add-on packages help accelerate market access through use-case-specific solutions, global regulatory content, a global team of subject matter experts and professional services.
- Accelerate time-to-market for products
- Reduce non-compliance risks that impact your ability to meet business goals and cause reputational damage
- Enable business continuity by digitizing your compliance process and building corporate memory
- Improve efficiency and enable your team to focus on business critical initiatives rather than manual tasks
- Save time with access to Compliance & Risks’ extensive Knowledge Partner network
- Definition on MDCG 2020-6 item 1.2 ↩︎
- Goland J. A., Algorithmic disgorgement: Destruction of artificial intelligence models as the FTC’s newest enforcement tool for bad data. Richm. J. Law Technol. XXIX (2023) found at https://heinonline.org/HOL/LandingPage?handle=hein.journals/jolt29&div=8&id=&page= on 20.05.2025. ↩︎
- FDA defines “locked” algorithm as an algorithm that provides the same result each time the same input is applied to it and does not change with use. Examples of locked algorithms are static look-up tables, decision trees, and complex classifiers. Found at the Proposed Regulatory Framework for Modifications to Artificial Intelligence/Machine Learning (AI/ML)-Based Software as a Medical Device (SaMD) – Discussion Paper and Request for Feedback https://www.fda.gov/files/medical%20devices/published/US-FDA-Artificial-Intelligence-and-Machine-Learning-Discussion-Paper.pdf (Page 3). ↩︎
- A collaborative effort involving EU national authorities, EMA, stakeholders and others.https://health.ec.europa.eu/medical-devices-topics-interest/combined-studies_en ↩︎
EU & UK Product Compliance: What’s Hot in 2025 & Beyond
Join us for expert insights into the latest developments, upcoming changes, and how to prepare for the evolving EU and UK regulatory landscape in 2025 and beyond.