Software as a Medical Device (SaMD) Compliance Strategies
THIS BLOG WAS WRITTEN BY THE COMPLIANCE & RISKS MARKETING TEAM TO INFORM AND ENGAGE. HOWEVER, COMPLEX REGULATORY QUESTIONS REQUIRE SPECIALIST KNOWLEDGE. TO GET ACCURATE, EXPERT ANSWERS, PLEASE CLICK “ASK AN EXPERT.”
The Software as a Medical Device market is racing toward $58.03 billion by 2030 – nearly doubling from $30.26 billion in 2024. Behind this explosive growth lies a regulatory gauntlet that separates market leaders from costly compliance failures. From AI-enabled diagnostics to remote monitoring platforms, SaMD products face an intricate web of evolving global requirements that can derail even the most promising innovations.
This blog decodes the regulatory lifecycle of SaMD products with actionable strategies for classification, cybersecurity, AI/ML considerations, and clinical validation. Whether launching your first medical software or scaling across markets, you’ll discover the compliance approaches that turn regulatory requirements into competitive advantages.
Table of Contents
- Understanding SaMD: Definitions and Classification
- The SaMD Regulatory Lifecycle
- Critical Compliance Pillars: Cybersecurity, AI/ML, and Clinical Evidence
- Regional Compliance Navigation
- Building Your Future-Ready Strategy
- FAQ: Common SaMD Compliance Questions
Understanding SaMD: Definitions and Classification
Before investing resources in compliance, proper classification prevents the costly missteps that plague 40% of initial submissions. The International Medical Device Regulators Forum (IMDRF) defines SaMD as “software intended to be used for one or more medical purposes that perform these purposes without being part of a hardware medical device.”
This distinction from Software in a Medical Device (SiMD) fundamentally shapes your regulatory pathway. SaMD functions independently – think diagnostic imaging analysis software – while SiMD operates within hardware devices like pacemaker control systems.
The IMDRF Risk Framework
The IMDRF framework evaluates SaMD across two critical dimensions. Healthcare Decision Information ranges from non-serious (low impact on patient outcomes) to critical (life-threatening condition decisions). Healthcare Situation considers whether use occurs in professional healthcare environments or patient settings outside clinical supervision.
This creates four risk categories from Class I (lowest) to Class IV (highest), directly determining documentation requirements and approval pathways. The FDA adopted IMDRF principles while maintaining its Class I, II, III structure. Class II typically requires 510(k) premarket notification, while Class III demands rigorous Premarket Approval (PMA). European regulation follows Rule 11 classification, emphasizing clinical evidence generation and comprehensive technical documentation regardless of risk level.
Understanding classification nuances prevents regulatory delays. A diagnostic algorithm informing treatment decisions qualifies differently than one providing general wellness information. These distinctions impact not just approval pathways but ongoing compliance obligations, post-market surveillance requirements, and market access timelines.
The SaMD Regulatory Lifecycle
Regulatory success requires viewing compliance not as a final hurdle but as an integrated development philosophy. The lifecycle encompasses strategic planning, compliant development, validation, market authorization, and post-market management.
Strategic Regulatory Planning
Early regulatory engagement prevents 70% of late-stage compliance failures. Pre-Submission meetings with the FDA or Scientific Advice procedures in the EU validate your regulatory strategy before significant resource commitment. These consultations clarify classification questions, clinical evidence requirements, and optimal submission pathways.
Key planning considerations include intended use precision – vague claims trigger elevated classifications – user environment analysis, global market strategy, and clinical evidence approach. Organizations navigating multiple regulatory frameworks benefit from harmonized development strategies that design studies and documentation to satisfy diverse regional requirements simultaneously.
Compliant Development Framework
IEC 62304 provides the foundational structure for medical device software development. This standard mandates software safety classification (Class A, B, or C), determining development rigor and documentation depth. Class A requires basic documentation, Class B demands enhanced risk management and architectural design, while Class C necessitates comprehensive validation and change control.
The standard requires five essential processes: software development planning, risk management activities, architectural design, configuration and change management, and problem resolution procedures. Modern agile methodologies can integrate with these requirements through “regulation-aware sprints” that incorporate compliance checkpoints without disrupting development velocity.
Validation Excellence
Validation confirms your software addresses intended clinical needs while verification ensures it meets specifications. For SaMD, technical functionality verification must align with clinical outcome validation. Risk-proportional approaches enable streamlined validation for low-risk applications while high-risk SaMD demands comprehensive testing covering normal use, foreseeable misuse, and edge cases.
Organizations implementing risk-based testing strategies report 60% reductions in validation time while maintaining safety standards through targeted protocols focusing resources on highest-risk components.
Critical Compliance Pillars: Cybersecurity, AI/ML, and Clinical Evidence
Three interconnected domains define modern SaMD compliance excellence: cybersecurity resilience, AI/ML regulatory navigation, and clinical evidence generation.
Cybersecurity Framework
Healthcare cybersecurity threats surged 123% in 2023, making robust security essential for both patient safety and regulatory compliance. The FDA’s cybersecurity guidance mandates comprehensive approaches spanning design, development, and post-market phases.
Pre-market requirements include cybersecurity device design considerations, Software Bill of Materials (SBOM) submission, risk-based controls, and vulnerability assessment. SBOM requirements became mandatory for FDA submissions in October 2023, encompassing commercial, open-source, and off-the-shelf components with version identification and hierarchical relationships.
Effective SBOM management requires automated tools tracking dependencies throughout development – manual maintenance becomes impractical for complex systems with hundreds of components. Post-market obligations include continuous monitoring, vulnerability remediation protocols, incident reporting, and regular security updates.
Medical device threat modeling must consider clinical workflow integration, patient data sensitivity, and healthcare system interoperability. SaMD-specific threats include clinical decision manipulation, patient data exfiltration, system availability attacks, and supply chain compromises. Security-by-design principles embedded throughout development reduce post-development retrofitting costs by 85%.
AI/ML Regulatory Navigation
AI-enabled medical devices represent 67% of recent FDA SaMD approvals, introducing unique regulatory challenges. The FDA’s Total Product Lifecycle (TPLC) approach shifts from traditional “point-in-time” approval to ongoing validation throughout the product lifecycle.
Good Machine Learning Practices (GMLP) address six critical areas: multi-disciplinary expertise integration, robust software engineering and security, training data management ensuring representative datasets, appropriate model selection and training, rigorous evaluation and performance monitoring, and model transparency providing adequate clinical decision explanations.
Predetermined Change Control Plans (PCCP) enable AI/ML systems to adapt while maintaining compliance. These plans pre-specify allowable changes, modification boundaries, and validation requirements for algorithm updates. Effective PCCPs reduce time-to-market for AI/ML updates from months to weeks while maintaining safety through proactive change management.
AI/ML validation extends beyond traditional testing to encompass algorithmic fairness, robustness, and interpretability. Validation must demonstrate bias assessment and mitigation across patient populations, robustness under diverse conditions, interpretability ensuring clinician understanding, and human factors evaluation assessing user interaction patterns.
Clinical Evidence Excellence
SaMD clinical evaluation follows three fundamental pillars. Valid Clinical Association establishes that your SaMD’s target condition, healthcare decision, and clinical management pathway create meaningful patient benefits. Analytical Validation proves your software accurately measures or detects the target condition. Clinical Validation demonstrates that SaMD outputs enable healthcare decisions improving patient outcomes.
FDA guidance increasingly emphasizes real-world evidence (RWE) offering advantages including larger sample sizes through electronic health records, diverse populations representing actual demographics, authentic clinical workflows, and continuous post-market data collection. However, RWE requires rigorous data quality controls and bias mitigation strategies for regulatory acceptability.
AI/ML systems introduce unique clinical evaluation challenges. Performance must be validated across demographic subpopulations to demonstrate fairness. Human-AI interaction validation must evaluate how healthcare providers interact with recommendations, including acceptance rates and override patterns. For adaptive algorithms, clinical validation must demonstrate that performance improvements maintain safety standards.
Regional Compliance Navigation
Global SaMD deployment demands understanding diverse regulatory landscapes with distinct requirements, timelines, and cultural considerations. The FDA emphasizes risk-based approaches with established 510(k) and PMA pathways, strong cybersecurity and AI/ML guidance, and relatively fast review timelines. European MDR requires comprehensive technical documentation, notified body involvement for most SaMD, and strong emphasis on clinical evidence with longer but predictable approval processes.
Asia-Pacific markets present unique considerations. Japan’s PMDA emphasizes clinical data from Japanese populations with unique AI/ML approval categories. China’s NMPA requires mandatory local clinical trials for most applications with data localization requirements and growing cybersecurity emphasis.
Strategic multi-regional approaches include sequential market entry targeting lead markets first, harmonized development designing studies satisfying multiple requirements simultaneously, and regional partnerships with local regulatory consultants navigating cultural nuances effectively.
Data sovereignty considerations significantly impact SaMD architecture. China, Russia, and India impose data residency requirements while GDPR creates complex transfer requirements. Plan architecture to accommodate regional data requirements from initial development rather than costly retrofitting.
Building Your Future-Ready Strategy
The SaMD regulatory landscape evolves rapidly, driven by technological advancement and changing healthcare delivery models. Future-ready strategies anticipate regulatory trends while maintaining current compliance excellence.
Regulatory trends indicate increasing adaptive frameworks embracing iterative approval processes, expanding international harmonization efforts, and growing real-world evidence integration. Emerging technologies including blockchain for data integrity, Internet of Medical Things integration, and digital therapeutics create new regulatory considerations.
Cost-Benefit Optimization
FDA submission costs range from $10,000 for 510(k) to over $2 million for complex PMA submissions, but hidden costs often exceed direct fees. Clinical study expenses can reach $500,000-$5 million depending on scope, regulatory consulting typically costs $200-400 per hour, and each month of delay can cost $100,000-$500,000 in lost revenue.
Smart optimization includes early regulatory engagement avoiding costly late-stage changes, risk-based validation focusing resources on highest-impact areas, regulatory precedent research leveraging existing pathways, and strategic partnerships with experienced regulatory consultants.
Strategic Implementation
Embed regulatory considerations into product development from conception. Balance regulatory investment with development resources through risk-based approaches and strategic advice utilization. Design systems and processes handling increased regulatory complexity as you scale and expand into new markets.
Companies with robust compliance frameworks achieve 40% faster regulatory approvals and 60% lower post-market compliance costs compared to reactive approaches. The organizations thriving in this landscape treat compliance not as a hurdle but as a competitive advantage building regulatory intelligence into their development DNA.
FAQ: Common SaMD Compliance Questions
- Q: What distinguishes SaMD from SiMD?
SaMD operates independently of hardware devices and performs medical functions through software alone – diagnostic imaging analysis, clinical decision support systems, patient monitoring applications. SiMD controls or operates hardware devices like pacemakers or MRI machines. When uncertainty exists, consult IMDRF guidance or seek regulatory advice. - Q: What’s the minimum documentation for low-risk SaMD?
Even Class I SaMD requires essential documentation including software requirements specifications, risk management records (ISO 14971), design controls, and verification/validation evidence. Documentation depth scales with risk, but focus on proportional approaches demonstrating safety without excessive bureaucracy. - Q: Can agile methodologies work for high-risk SaMD?
Yes, through careful integration with IEC 62304 requirements. Map regulatory milestones to sprint cycles, maintain continuous documentation, and implement risk-based validation strategies. The key is embedding compliance within agile workflows rather than treating them separately. - Q: How do PCCPs affect AI/ML development timelines?
PCCPs accelerate AI/ML deployment by pre-approving modification categories. Initial PCCP development adds 2-4 months but enables subsequent algorithm updates within weeks rather than months. Consider PCCP investment essential for any AI/ML system requiring regular improvements. - Q: What cybersecurity standards apply to SaMD?
Primary standards include ISO/IEC 81001-5-1 for health software security, FDA cybersecurity guidance, and EU MDR cybersecurity requirements. Implement security-by-design principles, maintain comprehensive SBOMs, and establish continuous vulnerability monitoring. Cybersecurity is an ongoing process, not a one-time requirement. - Q: When do software updates require regulatory submissions?
Updates affecting safety, effectiveness, or intended use typically trigger regulatory review. Minor bug fixes and usability improvements usually don’t require submissions. Significant algorithm changes, new clinical indications, or modified user interfaces often require regulatory evaluation. Maintain detailed change impact assessments supporting regulatory decisions. - Q: How long does SaMD regulatory approval take?
Timelines vary by region and complexity. FDA 510(k) reviews typically take 3-6 months, while PMA processes require 10-12 months. EU MDR submissions often take 6-12 months depending on notified body involvement. Plan for longer timelines and use pre-submission meetings optimizing approval strategies. - Q: What’s the ROI of comprehensive compliance strategies?
While upfront compliance investment seems substantial, comprehensive strategies reduce long-term costs through faster approvals, fewer regulatory challenges, and stronger market positioning. The companies that thrive treat compliance as a competitive advantage, building regulatory intelligence throughout their development process and creating systems that scale with growth ambitions.
Navigating SaMD compliance successfully requires strategic integration of compliance excellence throughout your product lifecycle. From initial classification through post-market surveillance, every decision impacts both regulatory success and commercial viability. The regulatory landscape will continue evolving, but with the right frameworks and strategic approaches, you can navigate complexity while accelerating innovation that improves patient outcomes worldwide.
Experience the Future of ESG Compliance
The Compliance & Risks Sustainability Platform is available now with a 30-day free trial. Experience firsthand how AI-driven, human-verified intelligence transforms regulatory complexity into strategic clarity.
👉 Start your free trial today and see how your team can lead the future of ESG compliance.
The future of compliance is predictive, verifiable, and strategic. The only question is: Will you be leading it, or catching up to it?
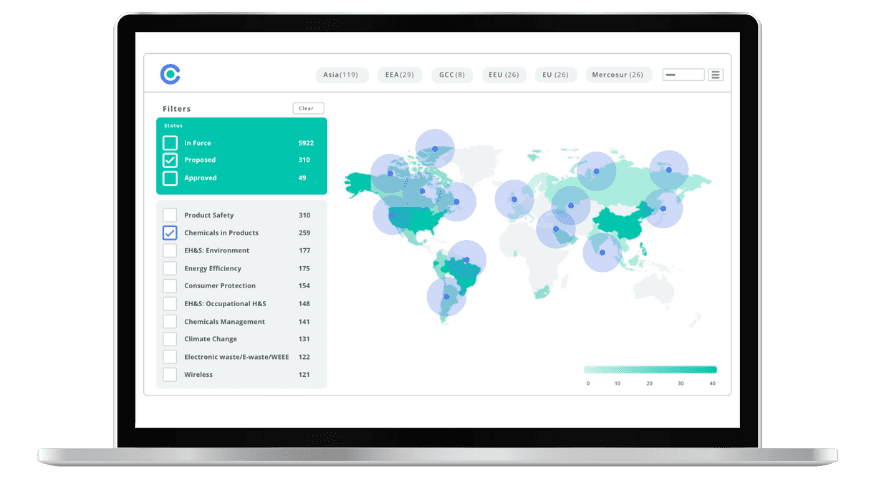
Simplify Corporate Sustainability Compliance
Six months of research, done in 60 seconds. Cut through ESG chaos and act with clarity. Try C&R Sustainability Free.